Research funded by Barts Charity has found your breath could give clues about blood cancer. This could enable the development of a special breath test that could spot blood cancer quickly and easily.
This has the potential to be a simple and low-cost way to detect blood – and be useful for areas with limited access to specialist equipment or expertise. This research is led by scientists at Barts Cancer Institute, based at Queen Mary University of London.
The challenges of diagnosing blood cancer
In the UK, around 40,000 people are diagnosed with blood cancer and around 16,000 people die of the disease each year. Diagnosing blood cancers can be challenging as early symptoms are often non-specific, such as fatigue and weight loss.
Diagnosis usually relies on specialised tests such as imaging scans or biopsies, which can be expensive or difficult to access in some regions.
Faster, low-cost and non-invasive test options could help diagnose blood cancers earlier, when treatment has a higher chance of success. They could also help monitor the disease and track how well treatments are working.
Using a breath test to diagnose blood cancer
“Previous studies have shown the value of using breath tests to detect lung cancer. But no one had ever investigated whether blood cancer cells release molecules that pass into the breath, despite the purpose of breathing being to exchange substances between the blood and the breath.”
Dr John Riches, Clinical Reader at Barts Cancer Institute, Queen Mary
In a study that we funded, published in HemaSphere, Dr Riches and his team demonstrate for the first time that a breath test could help detect blood cancers. Using Breath Biopsy®, a breathalyser technology developed by Owlstone Medical, the team collected breath from 46 people with blood cancer and 28 healthy people. They then analysed the chemical fingerprint of the breath, searching for tens of thousands of molecular fragments using a technique called mass spectrometry.
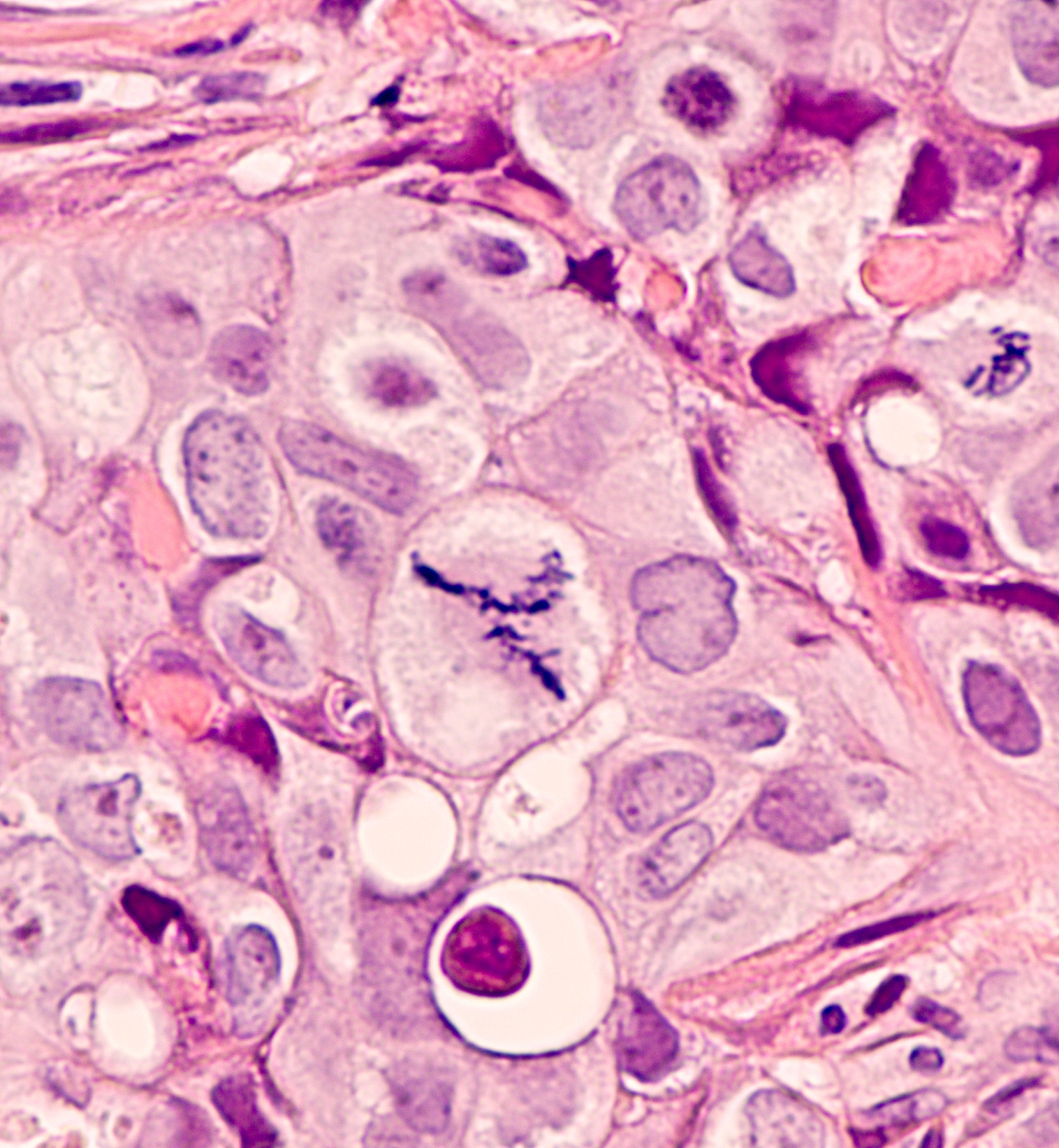
The researchers showed that people with high-grade lymphoma, an aggressive type of blood cancer that affects the lymphatic system, have significantly increased levels of certain molecules in their breath compared with healthy people. These include molecules that are produced when fats in our cells are damaged by a process called oxidative stress, which is known to play a role in the development of cancer.
Potential impact of this finding
The simplicity, affordability and portability of breathalyser devices compared with conventional diagnostic methods also means they could be used anywhere in the world. This could particularly benefit low-resource settings that lack access to scanners or specialist histology staff and facilities, such as in rural areas or developing countries.
“In future, rather than sending patients away for costly scans and waiting for test results, doctors may be able to conduct a quick breath test in their clinic room and potentially have the results within a few seconds.”
Dr John Riches
Further research is needed to develop an effective blood cancer breath test. The team will work to better understand the biology governing the production of the airborne molecules detected in patients’ breath, and which specific types of lymphoma are most reliably detected using this method. This will aid the development of more specific and sensitive tests, which the researchers hope could shorten the current 10 minutes required for breath collection to just a few seconds.
“In funding this study, we are backing innovative research that has the potential to make blood cancer diagnosis faster, more accessible, and less invasive. This has the potential to save lives.”
Victoria King, Director of Funding & Impact, at Barts Charity